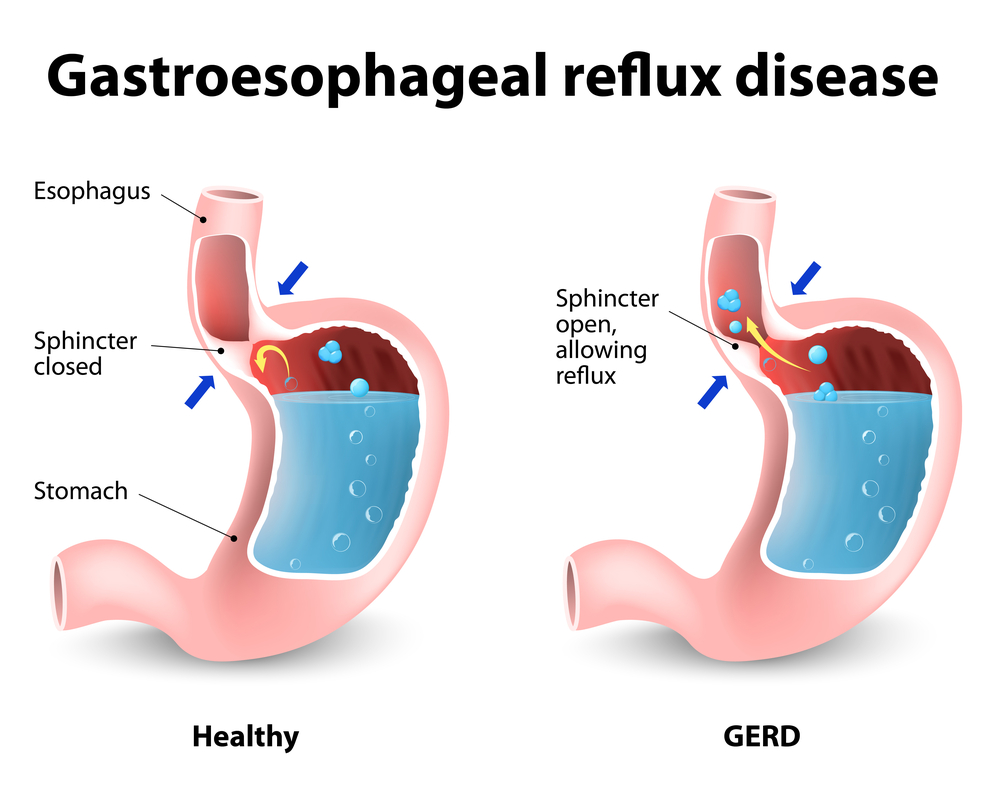
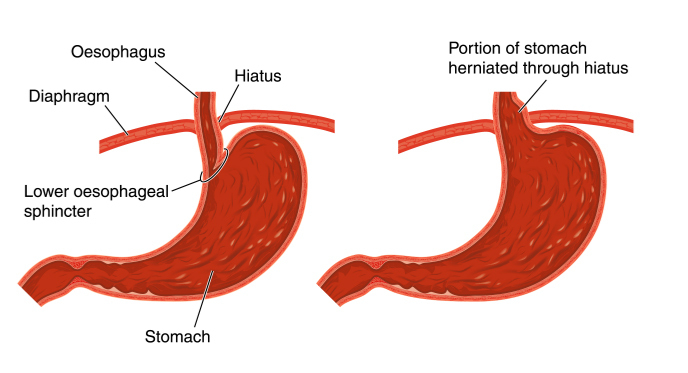
Gastroesophageal reflux disease, or GERD, is a digestive disorder that affects the lower oesophageal sphincter (LES), the ring of muscle between the oesophagus and stomach. Doctors believe that some people suffer from GERD due to a condition called hiatus hernia.
Some Facts:
- A chronic digestive disease where the liquid content of the stomach refluxes into the oesophagus.
- Common (More than 20,000 cases per year in UK)
- Rarely requires lab test or imaging
- Common for ages 50 and older
- Family history may increase likelihood
- Symptoms of severe chest pain & nausea
Factors contributing to GERD
Dietary and lifestyle choices may contribute to GERD. Certain foods and beverages, including chocolate, peppermint, fried or fatty foods, coffee, or alcoholic beverages. Studies have also shown that cigarette smoking relaxes the LES. Obesity and pregnancy can also play a role in GERD symptoms, pushing the stomach upwards releasing HCL into the oesophagus.

Digestion
Digestion happens in the digestive system, which begins at the mouth and ends at the anus.
After we swallow, our food passes through these organs in turn:
- oesophagus or gullet
- stomach
- small intestine
- large intestine.
In normal digestion, the lower oesophageal sphincter (LES) opens to allow food to pass into the stomach and closes to prevent food and acidic stomach juices from flowing back into the oesophagus. Gastroesophageal reflux occurs when the LES is weak or relaxes inappropriately, allowing the stomach’s contents to flow up into the oesophagus.
Hiatus hernia
Some doctors believe a hiatus hernia may weaken the LES and increase the risk for gastroesophageal reflux. Hiatus hernia occurs when the upper part of the stomach moves up into the chest through a small opening in the diaphragm (diaphragmatic hiatus). In some cases, people may not have heartburn or reflux, but they are at a higher risk. If symptoms are severe your Doctor may recommend surgery to reduce the size of the hernia or to prevent strangulation (twisted in a way that cuts off blood supply.
Treatment
- Decreasing the size of portions at mealtime
- Eating meals at least 2 to 3 hours before bedtime may lessen reflux by allowing the acid in the stomach to decrease and the stomach to empty partially.
- Lose weight.
- Stop smoking
- Elevating the head of the bed on 6-inch blocks to minimize reflux of stomach contents into the oesophagus.
- Do not prop yourself up with pillows! that only increases pressure on the stomach.
Treatment: Medication
Antacids can help neutralize acid in the oesophagus and stomach and stop heartburn. Long-term use of antacids, can result in side effects, including diarrhoea, altered calcium metabolism (a change in the way the body breaks down and uses calcium), and build-up of magnesium in the body. Chronic reflux may be prescribed H2 blockers, which inhibit acid secretion in the stomach. Proton pump inhibitor (or acid pump), inhibits an enzyme (a protein in the acid-producing cells of the stomach) necessary for acid secretion.
If acid reflux continues you may be recommended to have an Endoscopy. This is a procedure for individuals with chronic GERD. By placing a small lighted tube with a tiny video camera on the end – to see if there is any inflammation or gastritis.
What If Heartburn or GERD Symptoms Persist?
GERD might actually be caused by too little stomach acid. (Hypochlorhydria and achlorhydria)

Common cause of low stomach acid is acid reducing drugs. The second most common cause is chronic inflammation of the stomach. If low stomach acid is confirmed, the underlying cause of the condition (PPIs, H. pylori-mediated or autoimmune-mediated gastritis, etc.) should be addressed wherever possible.
Decrease of stomach acid with increasing age?
The human requirement for vitamins, minerals and other nutrients remains relatively constant throughout adult life. Our ability to properly digest food and absorb vital nutrients declines with advancing age. One of the most common age-related causes of impaired digestive function is the reduction of hydrochloric acid produced by the stomach. Hydrochloric acid (HCl) is an important gastric secretion that enables the body to break down proteins, activate important enzymes and hormones, and protect against bacterial overgrowth in the gut.
Symptoms of low stomach acid
Are similar to GERD so easy to misdiagnose as they include heartburn, indigestion, and bloating, among others. In the stomach, digestion begins with the release of a number of gastric secretions, including HCl, pepsinogen and a protective mucus coating. Normally the stomach contains enough free hydrochloric acid (HCl) to maintain a constant stomach acidity of between pH 1 and 2. If you don’t have enough stomach acid food can remain in the gut and ferment which can lead to GERD like symptoms.
Heartburn is a frequent symptom of low gastric acid.
Traditional approach of treating heartburn is to suppress gastric acid by taking antacids or medication. If you are really suffering from low stomach acid this is the opposite of what should often be done and may worsen the problem by suppressing gastric acidity when it is needed and promoting it (rebound phenomenon).
Book in with a Nutritional Therapist. They will discuss your symptoms and may suggest an HCL challenge test to determine if you have low stomach acid. Do not do this without supervision or if you are taking any medication.
Key Points
- Healthy digestion and absorption of nutrients is dependent upon the secretion of gastric acid.
- When gastric secretions are reduced the result can lead to nutritional deficiencies and a variety of chronic disorders.
- Low secretion of gastric acid can also allow orally ingested pathogens to prevail and contribute to their overgrowth in the stomach and small intestine.
- HCl supplementation is a safe and effective means of restoring normal gastric levels, if supported by a trained health professional like a Nutritional Therapist
- They will work closely with you to determine if you suffer with high or low stomach acid
Fiona Waring
Dip Nut, BSc.(Hons), MSc PHN, ANutr
Nutritional Therapist
M: +44 07957 267 964
eatyourgreens@fionawaring.com
‘Registered with the Association for Nutrition – www.associationfornutrition.org
Protecting the public and promoting high standards in evidence-based science and professional practice of nutrition.’